Did That Really Happen? Mid-life Interpretations & Confessions
June 30, 2021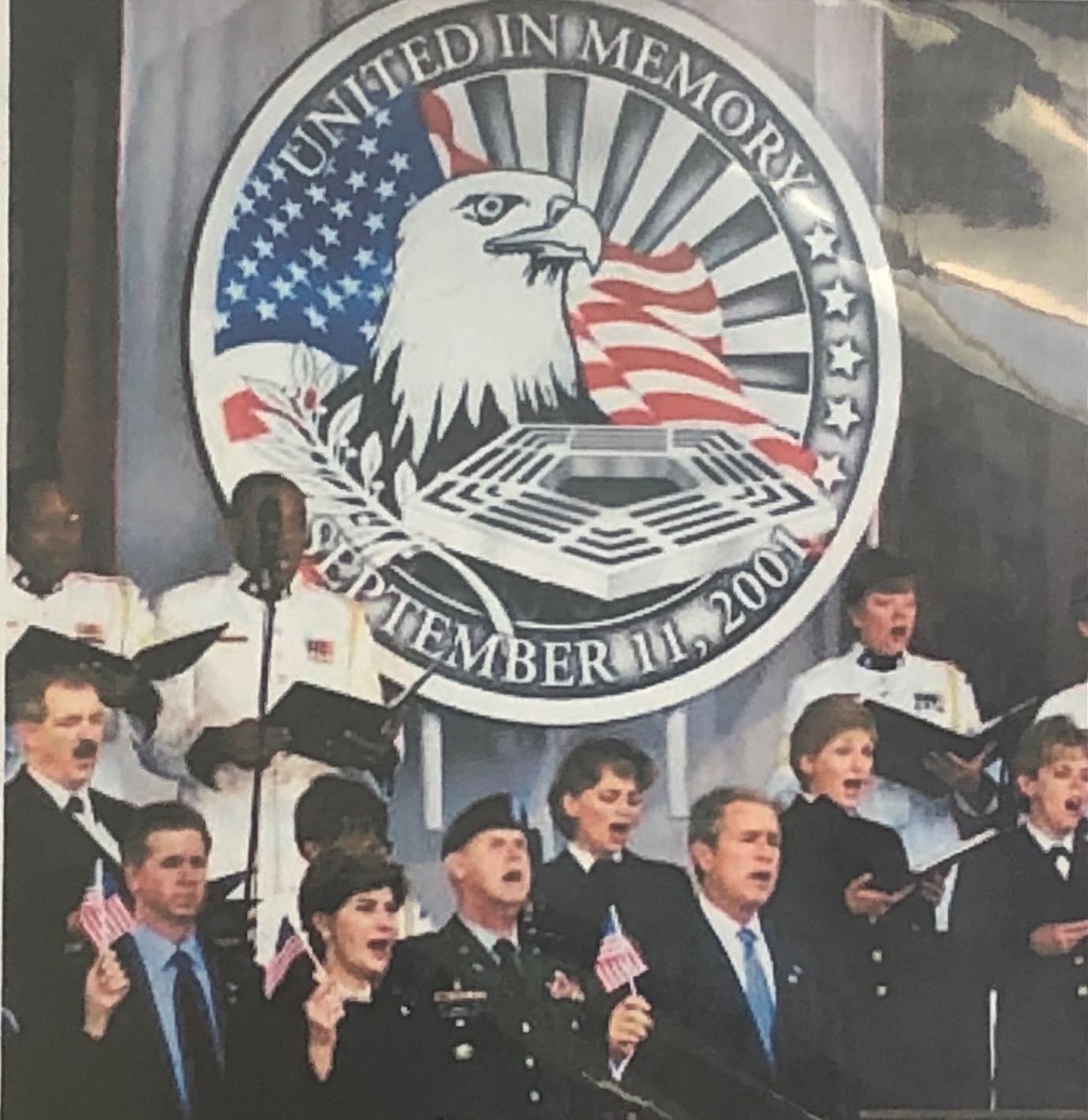
20 Years: Reflections and Healing
August 31, 2021One of my greatest joys is when a young professional reaches out to let me know they have decided to study what is called psycho-oncology—an interdisciplinary field at the intersection of the physical, psychological, social, and behavioral aspects of the cancer experience for patients, survivors, and caregivers.
Those are substantial words to essentially say that cancer tends to wreak holy havoc on one’s body and mind, not to mention the impact it has on caregivers who are often just as frightened and confused as the ones experiencing cancer.
About two years ago, a delightful woman, Stephanie Bennett, attended a Cancer Center Lunch and Learn talk I gave at the University of Colorado Anschutz Medical Campus. As she explains it, she was too emotional to introduce herself afterward; however, she reached out later to let me know her discovery of psycho-oncology had been a life-changing event. We became close friends, and she is now pursuing a Master of Social Work degree at the University of Denver’s Graduate School of Social Work. Earlier this year, I asked if she would collaborate with me on an educational blog post about the whats and whys of psycho-oncology, and she graciously agreed. Please meet the lovely, dedicated, and brilliant Stephanie Bennett in Q&A format. Thank you, Steph! Learn more about, and connect with her, here: https://www.linkedin.com/in/stephaniejbennett1/
Quick overview of where you grew up, your undergrad degree and what brought you to Denver
I was born in Montreal, Quebec, and moved with my family to the U.S. when I was quite young. I grew up in Rockford, Illinois, with my parents and two older brothers. I earned my Bachelor of Science in Psychology and Cognitive Science (double major) from Minnesota State University in 2014 and relocated to Denver soon after graduation.

Why were you attracted to psycho-oncology?
Like most, I have had several people in my life impacted by cancer. In watching their journeys, I began to recognize the dearth of psycho-social resources available to cancer patients and their loved ones. I was drawn to psycho-oncology after witnessing the lack of support available to individuals not only going through treatment but throughout the entire course of their cancer experience (from diagnosis through treatment into survivorship). From the first time I heard Diane speak at an event at the University of Colorado and read her book, The Unlikely Gift of Breast Cancer, I felt like I had found my calling—Diane put into words the feelings and concerns I observed in family members and friends during their cancer journey. I feel compelled to make a difference in the lives of patients and their families and strive to one day ensure nobody facing cancer feels lost nor alone.
Please explain why you have selected an educational path that allows you the maximum flexibility for clinical work and research.
Currently I am a graduate student in the Graduate School of Social Work at the University of Denver working toward becoming a licensed clinical therapist with a focus on oncology and chronic health conditions. After working in a research setting for many years with individuals with long-term health conditions including cancer, spinal cord injury, and traumatic brain injury, I began to feel a disconnect between the work I was doing, and the impact made on the lives of patients. Bringing research “from bench to bedside” to directly make meaningful change in the lives of patients takes time, and people need our help now. By earning my graduate degree in social work, I will learn tools to help patients and their families through the emotional and psychological demands brought on by cancer as well as provide essential resources necessary to decrease the burden brought on by disease.
Share what classes you have taken/will take and are required to become a licensed clinical therapist – what are your favorites and least favorites? Why?
Thus far in my graduate career I have completed courses in Psychotherapy, Psychopathology, Clinical Assessment, Personality Assessment, and Ethics and Professional Issues, among others. In the coming months I will take courses including Clinical Social Work Skills, Assessment of Mental Health Across the Lifespan, Clinical Social Work Theory and Practice, Mental Health and Health Care Policy, and will begin my first of two community-based internship placements. I am most excited for my upcoming work in the community through internship and work post-graduation. Learning theory, assessment, and the ethics and factors to consider when working with patients is extremely interesting and rewarding, however I feel nothing compares to actually being in the field working 1-1 with an individual or family!

Of the cancer patients/survivors/caregivers you have worked with already, what are your takeaways?
In both my professional and personal life, I have had the opportunity and privilege to work with and get to know a wide variety of cancer patients, survivors, caregivers, families and loved ones, and have learned something from each of them. Cancer impacts each individual differently. Furthermore, cancer is intricate and often works in strange and unexpected ways.

Through my time working at the University of Colorado Cancer Center, I have found it is incumbent on the patient to advocate for themselves and to make their needs known. Married to this is the idea that it often takes a village to face cancer. Patients take so much support from their network of people—medical professionals such as doctors and nurses, imaging specialists and surgery techs, as well as family members, friends, co-workers and colleagues, loved ones and other cancer patients and survivors—thus it is vital to tap into supports during challenging times. In addition to this large and varied group of supporters, patients still all too often report feeling alone, unsure of what to do next nor who to ask, wondering what resources may be out there to support them, and wishing for someone—anyone—to understand something about their journey they haven’t been able to reach anyone about.
What makes cancer-related physical and psychological trauma unique?
Cancer is a word that strikes fear into the hearts and minds of many. Its nature and behavior are still in many ways a mystery to us. Despite many significant advancements in the understanding of cancer over the years, the relative unknowns about cancer make it a black box that take away the comfort and security of life pre-cancer. The trauma brought on by cancer looks different in each individual and poses unique challenges to everyone touched by the diseases. As Diane writes in The Unlikely Gift of Breast Cancer, “cancer is inconvenient, inconsiderate, and extraordinarily covert” (p. 77).
Please explain where our healthcare system is at right now in terms of offering and encouraging those impacted by cancer to care about the psychological impact. What works? What doesn’t?
Psychological care is fortunately on the rise in the United States. Organizations such as the National Alliance on Mental Illness (NAMI) work tirelessly to lessen the stigma surrounding mental illness and reaching out to mental health professionals such as therapists, counselors, psychologists and psychiatrists. Despite this effort, many individuals still do not feel comfortable reaching out for help. Additionally, many communities lack an adequate supply of mental health providers with availability (plus there is often a lack of providers specialized in treating patients with long term health conditions such as cancer). Insurance and cost concerns are often another barrier to receiving care in that many insurance companies may only cover a limited amount of visits and/or certain providers (which may not encompass a preferred provider or a specialist such as an oncology social worker or psycho-oncologist). If an individual opts to pay out of pocket for visits with a provider not covered by insurance, or if they are uninsured, costs can inhibit ongoing, continued care which is frequently more appropriate than short-term treatment courses.
Please share why you believe mental health needs need to be addressed immediately after a person receives a cancer diagnosis. What do you think an ideal team approach should look like?
In a perfect world, I feel that newly diagnosed patients should be contacted by a medical health professional immediately after the dreaded “cancer call.” Just like regular meetings with medical staff such as nurses, oncologists, and surgeons, patients should have the option to visit with a psychosocial provider of their choosing (a psychologist or social worker, therapist, etc.) who they can speak to in a safe and confidential environment about anything related to their cancer experience. This specialist can help see to the needs of patients preemptively rather than having a patient wait until a problem arises to seek out necessary support. I would be remiss if I didn’t include the caveat that some individuals may feel they don’t feel the need to have a relationship with a counselor or other professional and that is absolutely fine as well. My life’s work is to ensure there are enough trained professionals in every community so anyone wishing to connect with a mental health professional in relation to their experience with cancer has the option available. Long term health conditions such as cancer are a unique stressor that bring about a variety of challenges both to the patient as well as their loved ones. Treatment teams must take it upon themselves to not only treat the disease, but to also treat the person, body and mind.
Well, there you have it! Brilliantly described by a compassionate student in the psycho-oncology field who believes (as I do) that the “team approach” to cancer needs to be expanded to ensure psycho-oncology has a permanent seat at the cancer treatment team’s table. Many cancer care centers are already embracing this concept—some more rapidly than others—but the winds of change have arrived, and leaders like Stephanie will carry us into the future. Woo-hoo! We are in good hands!
Before I go, last month a podcast I recorded earlier this year went live on Frank Zaccari’s Life-Altering Events series. Frank took a particularly compelling approach to why I am passionate about the bizarre combination of electric airplanes and psycho-oncology, and it’s one of my most favorite interviews so far. Listen and watch here:
I am working on a special treat for you next month, in recognition of the 20th anniversary of 9/11. Many of you know that my husband, Rene, was at the Pentagon that awful day, but there’s way more to the story than what I wrote about in The Unlikely Gift. Please be sure to tune in.
My thanks again to Stephanie Bennett for her courageous passion to help those impacted by cancer, and for her willingness to collaborate on this post. If you know of someone interested in psycho-oncology, either as a receiver of care or as a care provider, I’d be grateful if you would share this post with them, which—like all my blog posts—are available on my website, DianeMSimard.com. Thank you!
Love and hugs,